Surgical Procedures
Surgical procedures are carried out under local anaesthesia in the rooms or if authorised
by your medical aid, under general anaesthetic in hospital.
Confirm your date and time of admission

Stop smoking for at least 48 hours before the operation
You are not allowed to drive for at least 24 hours after undergoing general anaesthesia.
Inform us if you suffer from any serious diseases, and or allergies.
Arrange an authorisation number beforehand from your medical aid.
The hospital will supply you with a gown and underwear to wear during the operation.
If a cold or influenza is contracted before the operation date, you should please bring it under our attention.
Avoid taking Aspirin, as this might lead to excessive bleeding and bruising.
If you are younger than 18 years your parent / legal guardian / spouse should accompany you to sign for your operation.

1. You need to be starved for all anaesthetics and sedation for your own safety. No food or liquids may be taken by mouth for at least six (6) hours before the anaesthetic or sedation.
2. This means if you are on the morning list nothing per mouth from midnight. If you are on the afternoon list a light meal before 7am the morning of surgery is allowed (toast or cereal with clear liquid, no fat or meat).
Post-surgery FAQ
How Soon Will I Recover after Surgery?
While the complete healing process will take a few weeks, the post oral surgery recovery period is relatively quick. It differs with every patient and the different types of surgeries. Dr. De Lange will provide you with a sick note, according to the severity of the procedure.
Minor Oral Surgery such as a single tooth extraction / biopsy: patient should be functional within 24 -48 hours.
Dental Implants – depending on the procedure, the number of implants placed, whether bone augmentation was required, 3-5 days should be sufficient to recover. However, a 2-week follow-up visit is required to check that healing around the implant is satisfactory.
Impacted wisdom teeth – patients require 5-7 days. It can take up to 3-month for the jawbone to fill up where the tooth was removed.
Facial Trauma and Reconstruction surgery: 6-weeks. 2- and 6-week follow-up visits will be required.
How much pain can I expect after surgery?
Many patients biggest fear about oral surgery is the pain that can be expected afterwards. How much pain you can expect after surgery can vary depending on how extensive the procedure was that you had done. Dr. De Lange will prescribe the pain medication necessary to help you recover comfortably. Pain after most oral surgery tends to be mild to moderate and in almost all cases can be managed with over-the-counter medication every 6-8 hours
How Long Will I Be Swollen After Surgery?
Mouth and facial swelling will generally be at its peak in the first two to three days. After that, the swelling will gradually go down. Generally, the swelling will be 80% gone in five to seven days. Remember to carefully follow the instructions given to you on the day surgery, to heal as quickly as possible.
Swelling of the gums around the implant is normal after implant surgery, and often the swelling worsens after the first day and peaks about 72 hours after surgery. When multiple implants are placed, swelling, and bruising of the face and neck can sometimes occur. If major swelling occurs that affects vision, the ability to swallow or open one’s mouth wide enough to eat and drink, the patient should contact Dr. De Lange immediately.
Will I Be Able To Eat After Surgery?
Yes, you can eat. You should always eat something before taking your pain medication and antibiotics to avoid nausea. We recommend that you drink plenty of cold liquids after surgery and follow a soft food diet for at least 2-weeks. Avoid hot foods as it will disturb initial clot formation in the extraction sites. Following the day of the surgery, it’s best to avoid crunchy foods such as popcorn, nuts, and potato chips which break up into little pieces and can get packed down into the extraction sites. If you had dental implants placed, please avoid chewing hard foods with the implant itself for 8 weeks or the healing of the implant will be compromised. The typical implant requires 12-20 weeks of rest from chewing to completely integrate into the jawbone and be ready for a crown.
What if food gets stuck in the extraction area after surgery?
Your active rinsing with the saltwater recipe provided will begin the day after surgery, and this will help remove any food particles that may be stuck. Rinse after every meal for at least 2-weeks.
Can I brush my teeth like normal after surgery?
On the day of your surgery, do not spit or rinse your mouth. On the day after oral surgery, you can brush your teeth as you would normally again. When brushing, be gentle in the extraction sites as they may be tender for a few days following the procedure. Brush as well as you can and rinse with the saltwater recipe to aid in healing (1/2 teaspoon table salt + ¼ t bicarbonate of soda in 250ml warm water) 3-5 times per day. The use of commercial mouthwash is not recommended during the healing period. Sometimes the doctor will prescribe a mouth rinse to be used twice a day after surgery for one week as well.
Will I Have Stitches in My Mouth?
In most cases, patients will have a dissolvable suture at the surgical site(s). Sutures typically take 5-15 days to dissolve. In most instances, the stitches are placed at the time of surgery simply to assist with initial control of bleeding and clot formation. This is especially true with wisdom tooth surgery and other tooth extractions. Loss of a stitch is not considered an emergency, even if it came out on the day of surgery. If your surgeon has performed a bone-grafting procedure and the stitches are coming out prematurely, please contact our office so that the doctor may determine whether you need to be seen on that day.
If I Feel Nauseous After Surgery, What Should I Do?
Post-operative nausea and vomiting may occur due to the after-effects of the general anaesthesia and/or the prescribed medications. Treat nausea the same as you would the flu, (e.g. start with sips of clear liquids like water, 7-Up, ginger ale, apple juice). If those stay down, then continue these fluids until the nausea has completely subsided. Also, it is best to stop taking the prescribed medications until the nausea has passed. If after the first few sips the vomiting returns, wait 2 hours, and start the fluids again. If the pain is quite intense, you may take painkillers such as Ibuprofen. If you still feel nauseous after 24 hours, please contact our offices.
I had oral surgery and I’m still bleeding. What should I do?
It is not unusual to notice small episodes of bleeding for several days after having teeth removed. You can bite on a damp black tea bag (not rooibos) for 10-15 minutes; the tannic acid in tea helps in clot formation. If your mouth is rapidly filling up with blood and the above measures are not helping to slow down the bleeding, call our office for assistance.
Minor bleeding after implant surgery is to be expected. Placement of a gauze pad over the surgical site with mild biting pressure over the site for 30-45 minutes should effectively stop the bleeding. In special cases, such as a patient with high blood pressure or someone who is taking blood thinners, the implant surgical site may bleed for up to 48 hours after surgery. Vigorous bleeding in which the mouth is filling up with blood is not normal after implant surgery, and the patient should contact Dr. De Lange immediately if this occurs.
Food consumed on the day of surgery should be soft and cool; hot food and liquids may cause increased bleeding and swelling. After the first day, a gradual return to normal diet is acceptable; however, solid food should NOT be chewed directly over the top of the newly placed implant. Small movements of the implant from chewing may disrupt the healing process and cause the implant to fail.
Can I exercise after oral surgery?
On the day of surgery, vigorous exercise is NOT recommended. Light activity such as walking or indoor house chores is acceptable. After the first day, the patient should be cautious when returning to high impact exercise or outdoor chores as these may increase swelling, bleeding, and pain. Just be aware that if you get your blood pressure up, the surgical site may begin to throb and ache. At which time you want to slow down and take it easy. Pain medication can also have side effects such as dizziness that will negatively affect exercise.
The healing abutment on my implant came loose, what now?
Occasionally the healing cap that was placed over the implant during surgery may become loose during the days or weeks following surgery. If this occurs, there is no cause for alarm.
Contact the office during business hours and arrange to be seen by the surgeon to replace or tighten the healing cap. Please do not wait longer that 24-hours as the gum will start to close over the implant.
Does my medical aid cover my oral surgery?
Many oral surgeries are covered by general medical aid plans; however, it is subject to available benefits and scheme rules. The best thing to do is get a pre-estimate of the procedure from Dr. De Lange and then contact your medical aid and see if the procedure, or some of the procedure, costs are covered by your plan
What are the little pieces of white sand in my mouth?
Bone Graft material. When you have a bone graft placed, Dr. De Lange always overbuilds the graft because he knows you will lose some of the graft. So, you may find pieces of what feels like grit or sand in your mouth for the first week or two of healing.
Should I stop taking aspirin or blood thinners before my surgery?
Most oral surgery procedures can be performed while patients are on blood thinners. Unless Dr. De Lange has given you specific instructions to do otherwise, please continue to take your medications as prescribed. If you are on Warfarin, we will need a recent INR test prior to surgery.
Surgical Removals (Wisdom and other teeth)
What exactly are wisdom teeth?
Wisdom teeth or third molars are the last teeth to erupt, usually between the ages of 17 and 25 years. Most people have four wisdom teeth, but it is possible to have fewer or more. It is generally accepted that teeth which remain completely buried or unerupted in a normal position will have to be assessed for their potential to cause harm.
Teeth become impacted due to a lack of space in the dental arch. Their eruption is therefore prevented by gum, bone, another tooth or all three. When teeth are impacted it is best to remove them, as they can cause problems e.g. tooth crowding, infections and pain.
What are the risks involved in removing wisdom teeth and other molars?
Sometimes the roots of the teeth are lying across the facial nerve that supply your lower jaw with sensation and care should be taken in removing the roots without damaging the nerve.
Should the teeth in the upper jaw lie very high up, the sinus floor could be opened when they are removed. If this happens during the operation, the surgeon will have to close the sinus by creating a flap out of the gums to close the area.
Please adhere to the following instructions as closely as possible, to ensure healing of the sinus: Don’t blow your nose for two weeks; If you must sneeze, then please sneeze through your mouth and nose simultaneously – don’t block your nose to suppress your sneeze! Avoid sniffing very hard. Only use your prescribed nasal spray if your nose feels blocked. If you use it every 4 to 6 hours as advised on the package insert, it will only be effective for 5 days.
How much pain will I have after the operation?
Swelling and pain can be expected for about five days and varies from person to person, with the second day usually being the worst. If the swelling, bruising and pain continue for more than five days it is best to book a follow-up appointment.
Post-operative care:
- An antibiotic, an anti-inflammatory Painkiller and anti-septic mouthwash will be prescribed by the doctor after the operation (please inform the doctor if you are allergic to penicillin). Finish your course of antibiotics and avoid consuming any alcohol while taking medication. Don’t wait until the pain becomes unbearable before taking your pain medication, because then you might need larger dosages to control your pain. Rinse twice daily with the prescribed mouth wash.
- After tooth extraction, it’s important for a blood clot to form to stop the bleeding and begin the healing process. It will help towards a speedy recovery and lead to less bone loss. The blood clot will have a greyish-brown colour after a day or two – this should not be removed, sucked out or fiddled with the tongue, as this will cause a dry socket. That is when the blood clot formed at the extraction site is dislodged and results in irritation and extreme pain.
- Should the wound start bleeding again, take a teabag (black English Tea), wet it under the tap and bite lightly onto it – the pressure of the bite and the tannin in the tea will stop the bleeding by helping the blood to coagulate.
- It is advised to put an ice pack on the side of your face to prevent excessive swelling. This should be done at twenty-minute intervals for the first day after the operation.
- The stitches will dissolve by themselves any time between 5 and 15 days.
- No fluids for at least 1 hour after the operation. Take pain medication immediately with minimal water.
- For 3 hours after the operation no warm fluids or any other food.
- Avoid lying flat on your back, as this might lead to facial swelling. Sleep on 3 pillows for the first 48 hours. This will reduce swelling and bruising.
- Do not smoke for at least 48 hours after the operation as it promotes bleeding and interferes with the healing process.
- Only consume soft foods for the first three days, avoid popcorn or any other food with pips, seeds or peels for a period of 3 weeks.
Very Important:
You should also rinse your mouth with warm salt water (1 teaspoon of salt and ½ teaspoon of bicarbonate of soda dissolved in 250ml of water) as often as your wish or at least after every meal, but do not spit as this promotes bleeding and may dislodge the blood clot, which may result in a dry socket.
Abscesses
What is a tooth abscess?
A dental/tooth abscess is a localised acute infection at the base of a tooth, which requires immediate attention from your dentist. They are usually associated with acute pain, swelling and sometimes an unpleasant smell or taste in the mouth. More severe infections cause facial swelling as the bacteria spread to the nearby tissues of the face. This is a very serious condition. Once the swelling begins, it can spread rapidly. The pain is often made worse by drinking hot or cold fluids or biting on hard foods and may spread from the tooth to the ear or jaw on the same side.
What causes an abscess?
Damage to the tooth, an untreated cavity, or a gum disease can cause an abscessed tooth. If the cavity isn’t treated, the inside of the tooth can become infected. The bacteria can spread from the tooth to the tissue around and beneath it, creating an abscess. Gum disease causes the gums to pull away from the teeth, leaving pockets. If food builds up in one of these pockets, bacteria can grow, and an abscess may form. An abscess can cause the bone around the tooth to dissolve.
Why can't antibiotic treatment alone be used?
Antibiotics will usually help the pain and swelling associated with acute dental infections. However, they are not very good at reaching into abscesses and killing all the bacteria that are present. The Maxillofacial and oral surgeon will want to remove infected tissue as soon as it is possible, to remove the source of infection and prevent future problems. They might use antibiotics to help them do this, but the physical removal and stopping of potential places for bacteria to hide and grow is very important.
How is an abscessed tooth treated?
Antibiotics may be prescribed to destroy the bacteria causing the infection. If the infection is not cured, a hole can be drilled into the tooth to drain the infection. If the root of the tooth is infected, a root canal treatment is the recommended procedure (this tries to save your tooth by taking out the infected pulp). An apicectomy will be performed as a last resort to salvage the tooth. If this is unsuccessful the tooth may require extraction.
What is an apicectomy?
An apicectomy is a minor procedure to remove the tip (apex) of the root of a tooth. This is only done if a root canal treatment has failed. The procedure may be carried out using either a local anaesthetic, with or without intravenous sedation, or a general anaesthetic in a hospital operating theatre. The choice between the methods will depend upon the degree of difficulty of the procedure, your medical history, and your personal preference.
During the procedure a small “window” is cut (with a scalpel) in the gum over the root of the tooth. Using a dental drill, the area around the end of the root is exposed to determine the amount of root that should be removed. This portion of the root is then removed with the drill. Any infected tissue is removed from around the end of the root of the tooth.
Apicectomies are not very successful and have a 30-40% failure rate that results in the removal of the tooth.
Dental Implants
The decision to proceed with dental implant treatment affects your overall health, appearance, and well-being. We want you to be fully informed about your treatment options and what is involved with the procedures. Please find a summary of the discussion with Dr. de Lange and the reception staff regarding your treatment plan for the placement of dental implants.
What is a dental Implant?
Dental implants are replacement, or substitute tooth roots, used to replace natural tooth roots in areas of the mouth where teeth are missing. It is important to replace the missing tooth as natural tooth roots are embedded in the bone, providing a stable foundation necessary to bite and chew. In essence, the bone holds the tooth roots in place and the roots preserve the bone. When teeth are missing, the bone that previously supported those teeth deteriorates. This process is called bone resorption. However, the bone can be preserved by replacing missing tooth roots with dental implants. Since the bone forms a strong bond to the implants, they can serve the same functions as natural tooth roots.
Dental implants are designed to be permanent; however, many factors contribute to the long-term success of implant treatment, such as home care and regular maintenance visits to the dentist.
The implants are placed in the bone using a gentle surgical technique. Depending upon the stability of the implant, it may or may not be completely under the gum tissue, if a healing abutment is placed. Following the implant placement procedure, the implants are left undisturbed for a period of 5 to 9 months so that the bone can grow around the implants to form a strong biological bond to them. During this bone “integration” phase, you could have some temporary replacement dentures made, so that you never have to be without teeth during treatment.
Implant retained Bridges and Denture:
Damage to the tooth, an untreated cavity, or a gum disease can cause an abscessed tooth. If the cavity isn’t treated, the inside of the tooth can become infected. The bacteria can spread from the tooth to the tissue around and beneath it, creating an abscess. Gum disease causes the gums to pull away from the teeth, leaving pockets. If food builds up in one of these pockets, bacteria can grow, and an abscess may form. An abscess can cause the bone around the tooth to dissolve.
What Is the Cost of Implant Treatment?
Antibiotics will usually help the pain and swelling associated with acute dental infections. However, they are not very good at reaching into abscesses and killing all the bacteria that are present. The Maxillofacial and oral surgeon will want to remove infected tissue as soon as it is possible, to remove the source of infection and prevent future problems. They might use antibiotics to help them do this, but the physical removal and stopping of potential places for bacteria to hide and grow is very important.
Is Dental Implant Treatment Covered by Medical Aid?
Medical Aid coverage of implant treatment depends on the individual policy. However, it is rare to receive any substantial coverage. Most plans are only designed to cover routine maintenance, emergencies, and basic care with an annual maximum allowable benefit on most plans. Even if an individual policy includes implants as a covered benefit, the amount of coverage is still limited to the annual maximum allowable. An apicectomy will be performed as a last resort to salvage the tooth. If this is unsuccessful the tooth may require extraction.
Authorisation of Procedure
Please note that it is your responsibility as the patient to contact your medical aid to confirm benefits, co-payments and obtain authorization. If your medical aid declines authorization for the hospital, please contact us to reschedule an appointment in the rooms.
Payment of Dental Implant Components
Dr. de Lange requires upfront payment of dental implant components prior to the surgery, unless your medical aid can confirm in writing that they will cover the full cost of the components. You will receive an email with a cost estimate for the components the week before your surgery.
Follow-up visits with Dr. de Lange will be scheduled as follows:
- 2-weeks after surgery at no cost. Dr de Lange will evaluate the healing of the gingiva around the implants and check for any infection.
- 2,5-months after surgery at no cost. Dr. de Lange will check that the healing abutments are still firmly attached to the implants.
- 5-months after surgery as per attached cost estimate. Dr. de Lange will remove the healing abutments / surgically remove any gum that cover the implants. He will then insert a special torque wrench to test how strong the implant integrated with the bone.
- You need to obtain a quote and schedule an appointment with your Dentist to take impressions and fit the crown / bridge / denture to the dental implants.
Orthodontic surgery
Why do I need Surgical exposure of Impacted Canines/Eye Teeth?
An impacted tooth simply means that it is “stuck” and cannot erupt into function.
The maxillary canines/eye teeth are the second most common tooth to become impacted. The canine/eye tooth is a critical tooth in the dental arch and plays an important role in your “bite”. The canine teeth are very strong biting teeth and have the longest roots of any human tooth. They are designed to be the first teeth that touch when your jaws close together so they guide the rest of the teeth into the proper bite.
Normally, the maxillary canine teeth are the last of the “front” teeth to erupt into place. They usually come into place around age 13 and cause any space left between the upper front teeth to close tighter together. If a canine/eye tooth gets impacted, every effort is made to get it to erupt into its proper position in the dental arch. 60% of these impacted teeth are located on the palatal (roof of the mouth) side of the dental arch. The remaining impacted eye teeth are found in the middle of the supporting bone, but stuck in an elevated position above the roots of the adjacent teeth or out to the facial side of the dental arch.
Why do I need Orthodontic surgery?
Damage to the tooth, an untreated cavity, or a gum disease can cause an abscessed tooth. If the cavity isn’t treated, the inside of the tooth can become infected. The bacteria can spread from the tooth to the tissue around and beneath it, creating an abscess. Gum disease causes the gums to pull away from the teeth, leaving pockets. If food builds up in one of these pockets, bacteria can grow, and an abscess may form. An abscess can cause the bone around the tooth to dissolve.
What can I expect after the surgery?
Antibiotics will usually help the pain and swelling associated with acute dental infections. However, they are not very good at reaching into abscesses and killing all the bacteria that are present. The Maxillofacial and oral surgeon will want to remove infected tissue as soon as it is possible, to remove the source of infection and prevent future problems. They might use antibiotics to help them do this, but the physical removal and stopping of potential places for bacteria to hide and grow is very important.
How soon after the surgery should I see my Orthodontist
Antibiotics may be prescribed to destroy the bacteria causing the infection. If the infection is not cured, a hole can be drilled into the tooth to drain the infection. If the root of the tooth is infected, a root canal treatment is the recommended procedure (this tries to save your tooth by taking out the infected pulp). An apicectomy will be performed as a last resort to salvage the tooth. If this is unsuccessful the tooth may require extraction.
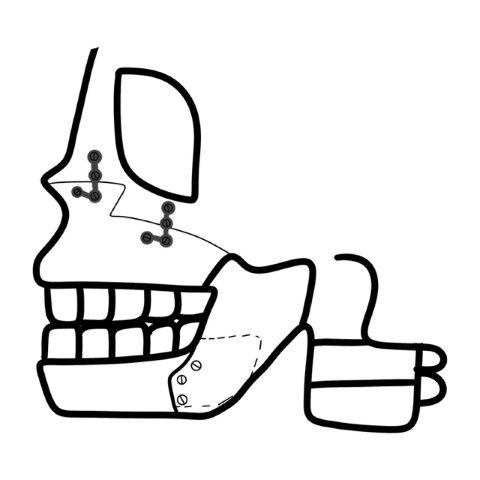
Orthognathic Surgery
What is Orthognatic Surgery?
Orthognatic surgery, also referred to an Osteotomy, is the cutting into your jawbone to change the structure of it. This occurs when it is not possible to correct your teeth and how they bite together with orthodontics alone. This happens because the bones of your face and jaws are out of balance with one another. Surgery (under general anaesthetic) will correct the relationship of the upper jaw to the lower jaw and will rectify these problems. One or more segments of the jaw can be simultaneously repositioned to treat various types of jaw deformities. Jaw surgery is best done after growth stops. The timing is usually ages 16 to 18 and older for females and ages 18 to 21 and older for males.
Why it's done?
Jaw surgery may help:
- Make biting and chewing easier and chewing better overall.
- Fix problems with swallowing or speech.
- Keep teeth from wearing out or breaking down.
- Fix bite fit or jaw closure issues, such as when the molars touch but the front teeth don’t touch. This is known as an open bite.
- Make the face look more balanced when there is a small chin, underbite, overbite or crossbite.
- Make the lips better able to close fully and comfortably.
- Ease pain caused by temporomandibular joint disorder and other jaw problems.
- Fix facial injuries or birth defects of the face and jaw.
- Ease obstructive sleep apnea.
What does the operation involve?
The operation is carried out almost entirely from the inside of your mouth so that there are minimal scars on the skin of your face. Rarely it is necessary to make a small incision on the skin of the face to allow the screws to be inserted. This is very small and usually only requires one stitch to hold it in place. If so, these cuts are placed where they’re less likely to be seen and are often very small.
Your surgeon makes cuts in the jawbones and moves them into the correct positions. After your surgeon moves your jaw into place, tiny bone plates, screws and wires may be used to secure the bones into their new positions. Rubber bands are often attached to braces. The screws, which are smaller than a bracket used for braces, usually combine with the bone structure over time, but some may be removed later.
The gum is stitched back into place with dissolvable stitches that fall out on their own. Sometimes extra bone is added to the jaw. To do this, your surgeon transfers the bone from your hip, leg or rib and secures it with plates and screws. Sometimes a bone graft can be taken from prefabricated bone grafts that don’t require bone to be taken from elsewhere in the body. Sometimes the surgeon reshapes the bone for a better fit.
Jaw surgery may be done on the upper jaw, lower jaw, chin or any mix of these locations.
Upper jaw surgery / Le Fort I,II,III Osteotomies
Surgery on the upper jaw, known as maxillary osteotomy, may be done to correct:
- An upper jaw that sinks in or sticks out too much.
- Crossbite.
- Too much or too little of the teeth showing.
- Open bite.
- A narrow upper jaw that’s too small compared with the lower jaw.
- Reduced facial growth of the middle of the face, also known as midfacial hypoplasia.
- Your surgeon cuts the bone above your teeth so that the whole top jaw, including the roof of your mouth and your upper teeth, can move as one unit. Your surgeon moves the jaw and upper teeth forward, backward, up or down until they fit properly with the lower teeth. In some cases, the surgeon can widen a narrow upper jaw during this surgery by making additional cuts through the roof of the mouth from the nose side of the upper jaw.
- An open bite occurs when too much bone grows above the molars. This causes what’s usually a flat, even surface to become angled. To fix too much bone growth, your surgeon shaves away or removes the excess bone.
- Once your surgeon lines up the jaw, plates and screws hold the bone in its new position.
Lower jaw surgery /BSSO
Lower jaw surgery, called mandibular osteotomy, can correct a lower jaw that sinks in or sticks out too much. The surgeon makes cuts behind the molars and lengthwise down the jawbone so the front of the jaw can move as one unit.
Then the surgeon can move the jaw forward or backward to its new position. Plates and screws hold the jawbone together as it heals.
Chin Surgery Genioplasty
A chin surgery, also known as a genioplasty or an inferior border osteotomy, can correct a small chin, also called a deficient chin. A small chin often can occur along with a lower jaw that sinks in too much.
Surgeons usually can change the jaw and restructure the chin during the same surgery. The surgeon cuts a piece of the chin bone on the front of the jaw, moves it forward, and secures it in a new position with plates and screws.
What can I expect after the operation?
Immediately after the operation your face will be swollen and will feel tight. Your jaws will be stiff, and you will find that you cannot open your mouth widely. The swelling and bruising will improve after about two days, as the second day is usually the worst.
You will only be able to have liquids for the first two days after surgery, but soon after that you should be able to progress to a soft diet. In a few weeks after surgery, you will be able to eat normal food again. The exact response to surgery is different in each case, but in general this is what you can expect.
After surgery, a healthcare professional gives you instructions. These instructions usually include:.
- What to eat, such as foods in liquid form for a period followed by a diet that is soft and easy to chew.
- How to keep your mouth clean.
- Not using tobacco.
- Not doing activities or lifting that takes a lot of energy or effort.
- How to take medicines to control pain.
- When to return to work or school, which is usually in 1 to 3 weeks.
- Initial jaw healing after surgery usually takes about six weeks, but full healing can take up to 12 weeks.
- After initial jaw healing ― at about six weeks ― your orthodontist can begin further aligning your teeth with braces. The entire orthodontic process, including surgery and braces, may take several years.
Once your orthodontist removes the braces, you may be given a retainer to hold your teeth in position.
Oral Pathology / Lesions in the mouth
What are lesions in the mouth?
The inside of the mouth is normally lined with a special type of skin (mucosa) that is smooth and coral pink in colour. Any alteration in this appearance could be a warning sign for a pathological process. The most serious of these is oral cancer. The following can be signs at the beginning of a pathological process or cancerous growth:
- Reddish patches (erythroplasia) or whitish patches (leukoplakia) in the mouth.
- A sore that fails to heal and bleeds easily.
- A lump or thickening on the skin lining the inside of the mouth.
- Chronic sore throat or hoarseness.
- Difficulty in chewing or swallowing.
These changes can be detected on the lips, cheeks, palate, and gum tissue around the teeth, tongue, face and/or neck. Pain does not always occur with pathology, and curiously, is not often associated with oral cancer.
Lesions are growths or sores that occur in the mouth. These can sometimes resolve themselves after a week or two, and in other circumstances they need to be removed surgically.
Different types of lesions
- self-induced lesions
- traumatic ulcers
- irritation fibroma
- nicotine stomatitis
- tobacco pouch keratosis
Self-induced lesions are due to habits such as scratching the gum with fingernails or lip, cheek and tongue biting. These usually require a biopsy to confirm the diagnosis.
Traumatic ulcers occur due to a trauma such as biting the lip, cheek, or tongue or from an irritation such as the sharp edge of dentures. Such lesions normally heal by themselves within 7-14 days however if they don’t, a biopsy is indicated.
Irritation fibroma is a lesion composed of dense, scar like connective tissue as a result of chronic trauma or habitual cheek biting or chewing. It is surgically removed and sent for a biopsy to confirm the diagnosis.
Nicotine stomatitis is a lesion induced by heavy smoking. Keratinization occurs resulting in raised red dots on the salivary glands. Tobacco pouch keratosis results in a white lesion from chewing tobacco. This lesion often disappears when tobacco is no longer chewed. In both nicotine stomatitis and tobacco pouch keratosis the smoking can cause an increased risk of squamous cell carcinoma (cancer), as well as an increased risk of caries, periodontal disease, attrition and staining of the teeth.
What is Oral Cancer?
Oral cancer occurs in the mouth, where the disease can affect the lips, tongue, cheeks and throat. It most commonly involves the tissue of the lips or the tongue, but can also occur on the floor of the mouth, cheek lining, gingiva (gums) or palate (roof of the mouth). Most oral cancers look very similar under the microscope and are called squamous cell carcinomas. These are malignant and tend to spread rapidly.
Who is most at risk for developing oral cancer?
Anyone can be affected by oral cancer, but it is most common in men over the age of forty.
Most cases of mouth cancer are linked to tobacco and alcohol. Chewing tobacco is very dangerous and if tobacco and alcohol are consumed together the risk is even greater.
Excessive exposure to sunlight increased the chance of developing lip cancer.
The human papilloma virus (HPV) plays a big role in the development of oral cancers.
Some early warning signs of oral cancer
• Any sores on the face, neck or mouth that do not heal in a month.
• Swelling, lumps or bumps on the lips, gums or other areas inside the mouth.
• White, red or dark patches in the mouth.
• Repeated bleeding in the mouth.
• Numbness, loss of feeling or pain in any area of the face, neck or mouth.
• Teeth that become loose or even fall out spontaneously might also be a warning sign.
Your dentist should normally do a mouth examination when he sees you every 6 months and any sign of cancer should be picked up.
How is cancer detected?
If you suspect you have cancer, or your dentist thinks that you may have it, you can come in and have a biopsy that is sent off to the pathology lab and it takes 2-3 working days to get the results. After we receive the results we will phone you and let you know the outcome, and advise you on what steps to take from there.
What treatment is available?
When the cancer is detected early the success rate for curing it is nearly 75%, unfortunately more than 50% of oral cancers are advanced by the time the cancer is detected. Surgical excision of the tumor is usually recommended if the tumor is small enough. Radiation therapy and chemotherapy would likely be used when the tumor is larger and has spread to the lymph nodes in the neck.
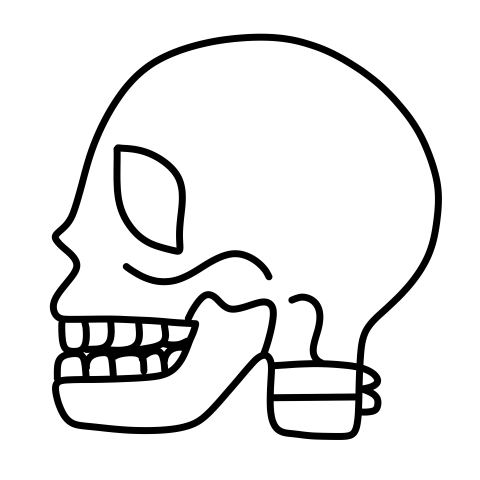
Temporomandibular Joint Disorder (TMJ)
The Temporomandibular Joint (TMJ) is the joint that connects the jaw. A TMJ replacement (TMJR) is akin to a joint replacement in other parts of the body, like the knee. Its purpose is to enhance the function of a deteriorated or injured joint by substituting the bony parts with a prosthetic joint. The procedure typically requires a brief hospital stay, followed by a recovery period.
What makes up my TMJ?
The TMJ can be considered a ball-in-socket joint. The ball (condyle) is a part of the lower jaw (mandible). The socket (fossa) is part of the skull. These two parts come together to form the moveable joint that you can feel when you place your fingers over the skin in front of your ears as you open and close your mouth. This structure is supported by ligaments and is influenced by the muscles of mastication.
When might I benefit from this procedure?
You may benefit from this implant if you suffer from one of the following conditions.
- Inflammatory arthritis (such as rheumatoid arthritis) of the TMJs not responsive to other treatment.
- Advanced osteoarthritis A.K.A bone to bone contact.
- Immobility of the joints (fibrous and/or bony ankylosis) not responsive to other treatment.
- Failed TMJ reconstructions using body tissue such as bone, muscle, or cartilage.
- Failed TMJ reconstructions using joints or other implants made from man-made materials.
- Loss of correct jaw position due to bone loss (resorption), trauma, developmental. abnormality, or tumour
- Missing TMJ due to birth defects.
When should this procedure not be performed?
This procedure should not be performed if you have one of the following conditions.
- Active or suspected infections in or near the TMJs
- Any mental or neuromuscular disorder that may cause the limitations and precautions for the use of this implant to be ignored
- Known allergy to any of the implant materials
What materials are in the prosthesis?
The components of this prosthesis are made with the same types of materials used for decades in orthopaedic surgery to successfully reconstruct
knees, hips, shoulders, elbows, and other joints of the body. The condylar component has a metal condyle made from cobalt-chromium-molybdenum.
This is attached to a metal implant body made from titanium alloy. This component is anchored to the lower jaw with titanium alloy screws. The fossa component has a durable medical-grade plastic surface made from ultra-high-molecular-weight polyethylene (also known as UHMWPE). This is
attached to a metal backing made from pure titanium. The component is anchored to the skull with screws.
How Are These Components Implanted?
The surgery used to implant these components is performed under general anaesthesia in a hospital operating room. Two incisions are made. The
condylar component is implanted through an incision below and behind the lower jaw. The fossa component is implanted through an incision in front
of the ear
What Are Possible Complications?
Complications may occur following placement of these implants and may require further treatment. The occurrence of a complication may be related to or influenced by previous surgical history or prior medical conditions. These complications include but are not limited to:
- Continued or increased pain levels or worsening of other present TMJ symptoms
- Infection
- Facial and jaw swelling after surgery usually lasting several days
- Bruising and discoloration of the skin around the eyes, ears, and jaw
- Temporary or chronic jaw muscle spasm
- Temporary or permanent facial muscle weakness resulting from motor nerve injury during surgery (The most common problems are an
inability to wrinkle the brow, raise the eyebrow, or fully close the eyelids.) - Temporary or permanent numbness of certain areas of the skin in the region of the joint and sometimes in more remote areas of the face
and scalp - Ear problems, including inflammation of the ear canal, middle or inner ear infections, perforation of the ear drum, temporary or permanent
hearing loss, ringing in the ears, and equilibrium or eustachian tube problems - Loss of joint mobility due to the development of scar tissue (adhesions), heterotopic bone, or ankylosis
- Dental malocclusion (improper bite) requiring bite adjustment, orthodontics, or reoperation
- Resorption or erosion of the glenoid fossa, mandible, or surrounding tissues
- Foreign body reaction or allergic reaction to implant components
- Wear, displacement, breakage, or loosening of implant components
- Functional compromise of the opposite TMJ when only one joint is being reconstructed
- Allergic reaction to any of the medications given during or after the surgery
- Objectionable scarring of the incisions
What Other Treatments Might I Need?
Due to the complex nature of your TMJ problem / the occurrence of a complication, you may require additional treatments including but not limited to:
- Extended physical therapy
- Bite splint therapy
- Restorative or reconstructive dentistry
- Orthodontics (dental braces)
- Orthognathic surgery (jaw repositioning surgery)
- Further reconstructive TMJ surgery
- Botox therapy if excessive grinding
What Can I Expect Following Surgery?
In the immediate post-operative period, you will be provided with the appropriate medication and care required for your recovery. Post-implantation
physical therapy is very important to achieving and maintaining optimum joint function. Dr Botha may recommend a jaw-exercising device for you.
You must follow the instructions regarding the use of that device to attain the maximum benefit from your surgery. It is also recommended that you
work with a physical therapist for a period post-operatively. Each case may have a different regimen in this regard, but most important is the continuous motion of the new joint to attain and maintain motion and function.
What Else Can I Expect?
Your diet will start as liquid, pureed, or even solid foods. This will depend on your particular circumstances regarding your TMJ. You may experience
“noises” from your new implants that include squishing, squeaking, clicking, and popping. These noises are not usual but may occur in some cases.
You may also notice stuffiness and/or a ringing sensation in your ears for a few weeks after surgery. This should subside over time. In order to implant these devices, certain muscles which assist in jaw function will have to be removed if they have not already been removed from a previous surgery.
This removal will reduce your ability to move your jaw from side to side and forward and down. Some of this motion may be regained, however, with
aggressive physical therapy. This implant will not allow you to have “normal” jaw function. A patient with a hip or a knee reconstruction cannot expect to be able to run in a race or participate in other sports that are strenuous on the legs. Similarly, a patient with a TMJ reconstruction should not expect to be able to eat hard, crunchy, or tacky foods without discomfort and risk of implant damage.
Long-term success with these joint prostheses may also be dependent on the physical demands placed on them. Excessive joint forces from grinding or “bruxing” teeth can lead to accelerated wear and fatigue resulting in early failure of this TMJ implant.
Will My Pain Be Reduced?
Even though many patients have experienced some relief from their symptoms, the amount of pain reduction will vary from patient to patient over
time. Patient data collected to date indicates that patients having undergone two or fewer previous surgeries experience less pain post-operatively
than those patients having undergone larger numbers of prior operations.
How Long Will This Reconstruction Last?
Even though these implants are fitted specifically to your anatomy, you should not expect them to last for a lifetime. While the expected life of a TMJ
implant is difficult to estimate, it is finite and may significantly differ for each patient due to the diversity of conditions seen in TMJ reconstruction.
These components are made from man-made materials which are placed within the body for the potential restoration of jaw function and reduction of pain. However, due to the many biological, mechanical, and physiochemical factors which affect these devices, the components cannot be expected to indefinitely withstand the activity level and loads of normal healthy bone. The longest study reviewed patients for 10 years with successful outcomes.
What Are the Alternatives To This Type Of Reconstruction?
Alternatives to this type of reconstruction include grafts of bone, soft tissue, or cartilage. The suitability of alternative treatments will depend on the
condition of the bones, cartilage, disc, ligaments, muscles, nerves, and blood vessels in and around your TMJs.
How Do I Care for And Protect My TMJ Implants?
- Inform us about other types of surgeries or dental procedures you intend to have after your TMJ reconstruction. We may want to prescribe
antibiotics to decrease the possibility of infection that could jeopardize the success of your implants. - Contact us if you have any problems related to your surgery or your TMJ implants.
- See us for prescribed follow-up visits. After the first year, it is important that you visit for annual check-ups.
- Follow post-operative instructions, especially those related to physical therapy.
- Continue to take medications and to follow the diet as prescribed.
- Avoid hard, crunchy, or tacky foods.
- Refrain from chewing gum.
- Avoid contact sports.
- Never place yourself at physical risk that may result in damage to your TMJ implants.
- Refrain from water sports and general strenuous physical activity for six weeks following surgery.
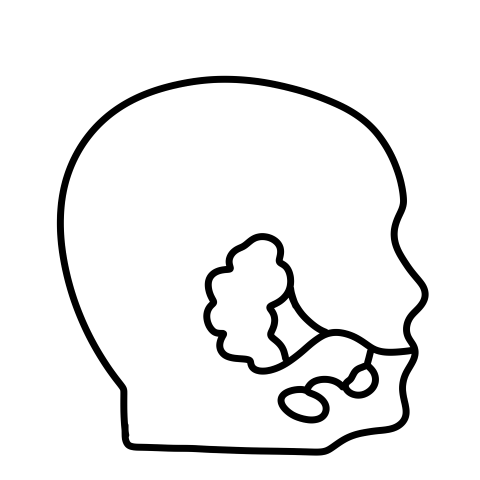
Salivary Gland Diseases
About Salivary Gland
Your salivary glands produce as much as a 1.5 litre of saliva each day. Saliva is important to lubricate your mouth, help with swallowing, protect your teeth against bacteria, and aid in the digestion of food. The three major pairs of salivary glands are:
- Parotid glands on the insides of the cheeks
- Sub-mandibular glands at the floor of the mouth
- Sublingual glands under the tongue
There are also several hundred minor salivary glands throughout the mouth and throat. Saliva drains into the mouth through small tubes called ducts.
Diagnosis and Symptoms
When there is a problem with the salivary glands or ducts, you may have symptoms such as salivary gland swelling, dry mouth, pain, fever, and foul-tasting drainage into the mouth. Salivary stones can interfere with the function of the salivary glands or block the ducts so they can’t drain saliva. When saliva can’t exit through the ducts, it backs up into the gland, causing pain and swelling that gets progressively worse. Unless the blockage is cleared, the gland is likely to become infected.
Bacterial infection of the salivary gland, most commonly the parotid gland creates a painful lump in the gland, and foul-tasting pus drains into the mouth. It is more common in older adults with salivary stones, but it can also happen in babies during the first few weeks after birth. If not treated, salivary gland infections can cause severe pain, high fevers, and abscess (pus collection). Bacterial infections generally cause one-sided salivary gland swelling. Cysts can develop in the salivary glands if injuries, infections, tumours, or salivary stones block the flow of saliva
Viral infections such as mumps, flu, and others can cause swelling of the salivary glands. Swelling happens in parotid glands on both sides of the face, giving the appearance of “chipmunk cheeks.” It usually begins approximately 48 hours after the start of other symptoms such as fever and headache. Other viral illnesses that cause salivary gland swelling could include for example the Epstein-Barr virus, cytomegalovirus, Coxsackievirus, and the human immunodeficiency virus.
Several different types of tumours can affect the salivary glands. They can be cancerous (malignant) or noncancerous (benign). The two most common tumours are pleomorphic adenomas and Warthin’s tumour. Pleomorphic adenomas most commonly affect the parotid glands, but can also affect the submandibular gland and minor salivary glands. The tumour is usually painless and grows slowly, are benign (noncancerous) and are more common in women than men. Warthin’s tumor is also benign and affects the parotid gland. Warthin’s tumor can grow on both sides of the face and affects more men than women.
Sjögren’s syndrome is a chronic autoimmune disease in which cells of a person’s immune system attack the salivary and other moisture-producing glands, leading to dry mouth and eyes. About half of people with Sjögren’s syndrome also have enlargement of the salivary glands on both sides of the mouth, which is usually painless.
Treatment
Treatment for salivary gland problems depends on the cause. For stones and other blockages of the ducts, treatment begins with the manual removal of stones, warm compresses, or sour candies to increase the flow of saliva. If simple measures don’t relieve the problem, surgery may be required. Surgery is usually required to remove large cysts and benign/malignant tumors. Some benign tumors are treated with radiation to keep them from coming back. Some cancerous tumors require radiation and chemotherapy. Other problems may be treated with medications only. For example, bacterial infections are treated with antibiotics. Medications can also be prescribed for dry mouth.
Trauma & Facial Injuries
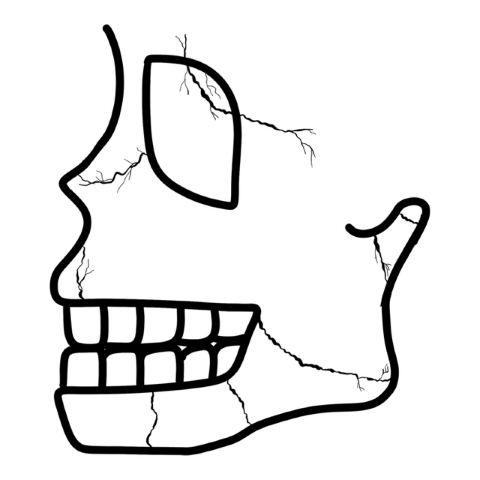
Facial Fractures, Injuries & Trauma
Maxillofacial injuries also referred to as facial trauma, encompass any injury to the mouth, face and jaw. There are a number of possible causes of facial trauma such as motor vehicle accidents, accidental falls, sports injuries, interpersonal violence, and work-related injuries. Typically, facial injuries are classified as either soft tissue injuries (skin and gums), bone injuries (fractures), or injuries to specific regions (such as the eyes, facial nerves or the salivary glands).
Injuries can vary from a dislodged (bumped out) tooth/teeth to complex combination of fractures of the bones of the face i.e. the lower jaw, upper jaw, palate, cheekbones, eye sockets and combinations of these bones.
What are the risks?
These injuries can affect sight, the ability to breathe, speak and swallow. Treatment often requires hospitalization and cannot be fixed immediately, as the swelling needs to subdue, and more serious injuries need to be treated first.
Bone Injuries
The fracture is treated under general anesthetic by placing plates and screws in place to hold the fractured bone segments together. This is done in a manner to ensure that the fewest number of scars are left on the face. This technique is called “rigid fixation” of a fracture. The relatively recent development and use of rigid fixation has profoundly improved the recovery period for many patients, allowing them to return to normal function more quickly. An attempt at accessing the facial bones through the fewest incisions necessary is always made. At the same time, the incisions that become necessary, are designed to be small and, whenever possible, are placed so that the resultant scar is hidden.
Once it is completely healed (this takes about two months) the plates and screws may be removed. Additional operations may be required after 6-12 months to ensure a pre-treatment facial structure.
Soft Tissue Injuries
When soft tissue injuries such as lacerations occur on the face, they are repaired by suturing. In addition to the obvious concern of providing a repair that yields the best cosmetic result possible, care is taken to inspect for and treat injuries to structures such as facial nerves, salivary glands, and salivary ducts (or outflow channels).
Once it is completely healed (this takes about two months) the plates and screws may be removed. Additional operations may be required after 6-12 months to ensure a pre-treatment facial structure.
Very Important:
Maxillofacial and Oral Surgeons are trained, skilled and uniquely qualified to manage and treat facial trauma. Injuries to the face, by their very nature, impart a high degree of emotional, as well as physical trauma to patients. The science and art of treating these injuries requires special training, involving a “hands on” experience and an understanding of how the treatment provided will influence the patient’s long term function and appearance.
After the fractures have been repaired, a healing time of between 4-6 weeks (often longer in more extensive cases) should be allowed. During this time the patient will need to follow a diet that is adapted to his/her own special circumstances and can differ from a strict fluid diet to a diet of semi-solid foods. Special attention to oral hygiene is essential. Physiotherapy is also valuable in the rehabilitation, especially in injuries of the jaw-joint or extensive skin and muscle injuries.
Once it is completely healed (this takes about two months) the plates and screws may be removed. Additional operations may be required after 6-12 months to ensure a pre-treatment facial structure.

